Housing First, Care Always
Hello! My name is Nivedha Satheeshkumar, and I recently moved back home to the Bay Area after going to school in Los Angeles. I am currently serving with the Permanent Housing Advanced Clinical Services (PHACS) Team within the Whole Person Integrated Care (WPIC) Department of the San Francisco Department of Public Health (SFDPH). I am eager to serve and grow in my position this year.
 Permanent supportive housing (PSH) is a program where tenants who have experienced homelessness are offered long-term leases in buildings that offer supportive services such as rental assistance, case management, and housing retention assistance, to name a few. For a person to be offered a PSH unit, there are no requirements detailing that an individual must be abstinent from substance use, have completed a residential training program, or must participate in services. This is in line with the Housing First Model, an evidence-based approach that emphasizes housing as a basic human right and a crucial first step toward recovery and stability. Within San Francisco, there are many PSH sites, typically centered in the Tenderloin and South of Market regions. The PHACS team works with the tenants and supportive services staff at 146 of these PSH sites to provide any short-term, non-urgent medical and behavioral health services with the ultimate goal of linkage to long-term, ongoing services. This is achieved with an interdisciplinary team of health workers, providers, behavioral health clinicians, pharmacists, and me, the Americorp member! Our program is activated upon receiving referrals from on-site case managers at PSH sites who will concisely describe what the resident needs support with. This mobilizes our team, which outreaches tenants directly at their residences and works with them to achieve their dynamic goals. In just 2024, PHACS received nearly 1,000 referrals from 129 buildings.
Permanent supportive housing (PSH) is a program where tenants who have experienced homelessness are offered long-term leases in buildings that offer supportive services such as rental assistance, case management, and housing retention assistance, to name a few. For a person to be offered a PSH unit, there are no requirements detailing that an individual must be abstinent from substance use, have completed a residential training program, or must participate in services. This is in line with the Housing First Model, an evidence-based approach that emphasizes housing as a basic human right and a crucial first step toward recovery and stability. Within San Francisco, there are many PSH sites, typically centered in the Tenderloin and South of Market regions. The PHACS team works with the tenants and supportive services staff at 146 of these PSH sites to provide any short-term, non-urgent medical and behavioral health services with the ultimate goal of linkage to long-term, ongoing services. This is achieved with an interdisciplinary team of health workers, providers, behavioral health clinicians, pharmacists, and me, the Americorp member! Our program is activated upon receiving referrals from on-site case managers at PSH sites who will concisely describe what the resident needs support with. This mobilizes our team, which outreaches tenants directly at their residences and works with them to achieve their dynamic goals. In just 2024, PHACS received nearly 1,000 referrals from 129 buildings.
In my role as a Care and Capacity Coordinator, I have the privilege of working closely with PSH residents to help them achieve their goals. My daily responsibilities often involve accompanying patients to their medical appointments and advocating for them, such as connecting them to community resources and, most importantly, linking them to long-term, accessible primary care. Beyond the tangible outcomes of this work, I deeply value the meaningful relationships I cultivate with my clients and the opportunity to offer companionship. Although spending time in crowded hospital waiting rooms or sitting for hours at the General Assistance office may seem mundane, these moments give me invaluable opportunities to connect with them. During these shared down-times, I learn about their hobbies, background, and personal stories, building trust and understanding. If not for these moments, I would’ve never learned about how one of them is in the process of writing a book about their life or how another used to own a cement company in Sacramento Valley.
 On the capacity-building side of my role, I scribe during clinical review sessions, during which a multidisciplinary panel makes recommendations to the Department of Homelessness and Supportive Housing (HSH) regarding resident placements within PSH buildings based on their clinical needs. Additionally, I focus on enhancing the support services available at PSH sites by educating on-site staff and providing them with tools and resources to better serve residents. These combined efforts aim to create an environment that fosters stability and growth for everyone involved.
On the capacity-building side of my role, I scribe during clinical review sessions, during which a multidisciplinary panel makes recommendations to the Department of Homelessness and Supportive Housing (HSH) regarding resident placements within PSH buildings based on their clinical needs. Additionally, I focus on enhancing the support services available at PSH sites by educating on-site staff and providing them with tools and resources to better serve residents. These combined efforts aim to create an environment that fosters stability and growth for everyone involved.
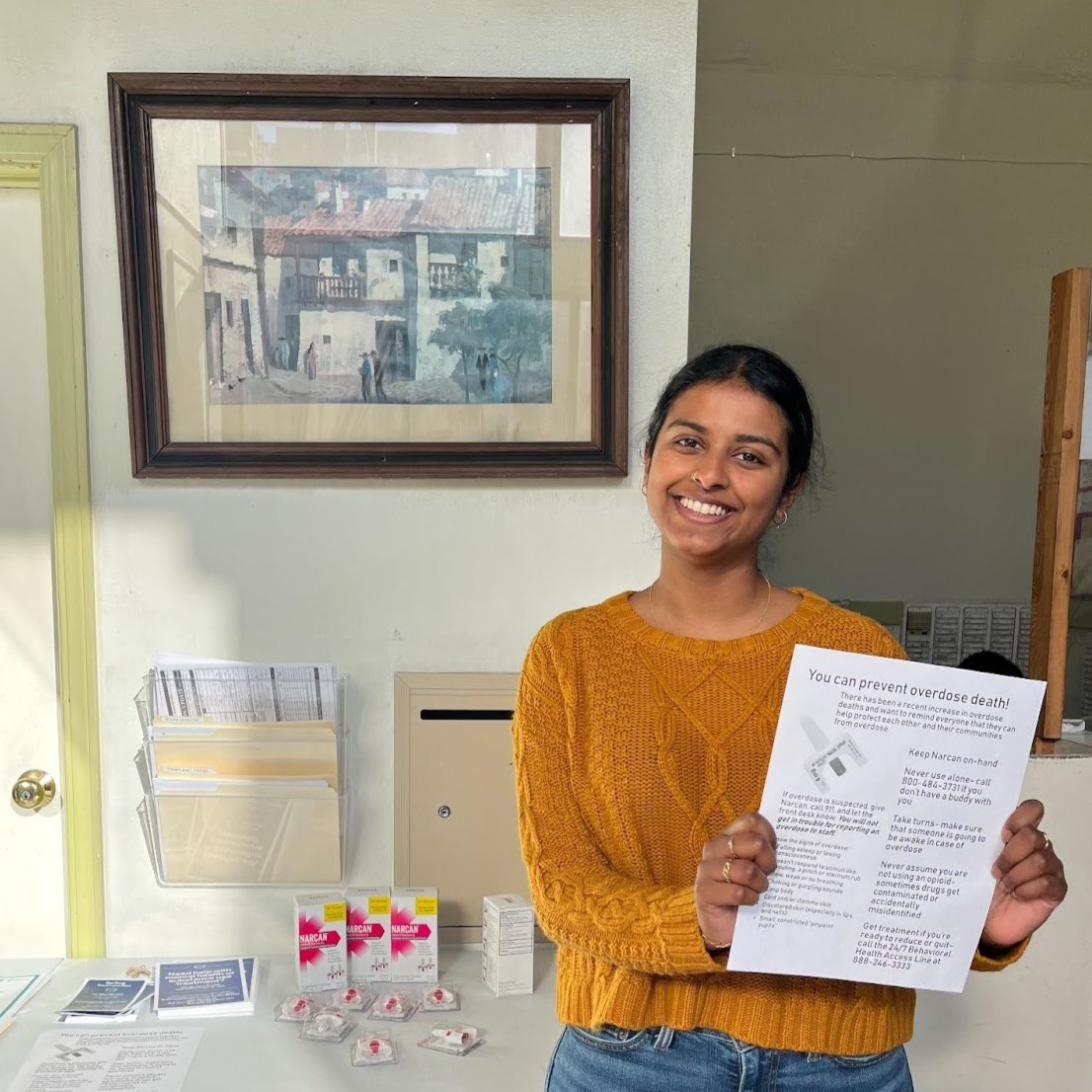
One of the most urgent and impactful areas of focus in my work has been addressing the disproportionate rate of fatal overdoses within PSH. Increasing access to medications for opioid use disorder (MOUD) is a critical component of these efforts. At PHACS, we work closely with on-site staff to educate them about overdose prevention and harm reduction strategies, ensuring they are well-equipped to respond to crises. We also directly engage residents by dropping in at community events to share information about MOUD and other available resources. When residents express interest, I help facilitate their intake at methadone clinics or connect them with prescribers who can prescribe various forms of buprenorphine, such as sublingual suboxone or long-acting injectables. MOUD is a life-saving intervention that not only significantly reduces the risk of overdose but also improves overall health and stability, which is why expanding access within PSH is such a priority for our team.
Working within PSH has been both challenging and incredibly rewarding. The complexity of residents' needs and their resilience inspires me every day. By providing individualized care, I hope to contribute to a system that empowers people to reclaim their health, housing, and sense of agency.
